Whoopi Goldberg, an Academy Award-winning actress, wanted to raise awareness about the dangers of pneumonia, so she invited her two doctors to her morning talk show “The View” to discuss the near-death experience the actress had with the illness earlier this year.
Doctors Jorge Rodriguez, MD (an internist and gastroenterologist) and Martin Greenberg, MD (a pulmonologist) said that Goldberg’s pneumonia and sepsis were so advanced when she arrived at the hospital that she had a “one in three” chance of dying from the infection.
Having assumed that her cough would go away on its own, Goldberg, 63, says she first noticed it in November of 2018. Whoopi “didn’t feel well” on February 6, so she called her business partner Tommy Leonardis to tell him she thought she needed to go to the hospital. He called her primary care physician, Rodriguez, who revealed to the audience what she told him: “Whoopi was so fast that I had a hard time following her.
Her lips were trembling and she was struggling to breathe.” After hearing that all she wanted to do was sleep, he became even more worried. “I fought the urge to squeak out a frightened sound but… I was worried she wouldn’t wake up because it’s hard to tell if someone who gives you hints like that is actually just tired, or if they’re about to pass out and that was it.”

For Goldberg to meet Greenberg, he had an ambulance take her to the hospital.
“Whoopi seemed to be in a bad place when I first met her. There were concerning signs: a high temperature, difficulty breathing, a fast heart rate, and a low oxygen level.”
They found that Whoopi Goldberg had pneumonia and septic shock. She had a pulmonary effusion that required two draining procedures. A radiologist placed a tube for an external chest drain after the effusion returned (see below).
After being admitted to the hospital for three weeks, she did not return to “The View” until April, and then only on a reduced schedule.
In an effort to encourage others to take charge of their health, Goldberg told her doctors, “It’s OK to go to the doctor because you don’t feel good.”
Goldberg said, “The crazy thing is people don’t take (pneumonia) seriously,” and she confessed that she didn’t at first. “All I did was (try to) push through it, and that’s obviously not an option. As a matter of fact, it’ll probably end your life. Passivity, inaction, and failing to check can be fatal.”
“In other words, pull yourself together and admit that you need medical attention because you’re not feeling well. You’d rather be here to complain about it than elsewhere.”
Introduction to Pneumonia
Pneumonia is an inflammation of the respiratory system caused by a bacterial, viral, or fungal infection that affects either the left or right side of the lungs and leads to the accumulation of fluid or pus in the alveoli or air sacs. Children younger than five, the elderly, and those with compromised immune systems due to HIV/AIDS, chemotherapy for cancer, or organ or blood and marrow stem cell transplant procedures are at higher risk of developing life-threatening pneumonia than others.
The majority of adult cases of pneumonia are caused by bacteria. Pneumonia is caused by many different kinds of bacteria. In the United States, bacterial pneumonia is most often brought on by pneumococcus bacteria, also known as Streptococcus pneumonia.
Pneumonia Caused by The Following Is Classified as “Atypical.”
The legionnaires’ disease-causing Legionella pneumophila. Legionnaires’ disease, another name for this form of pneumonia, has been responsible for devastating epidemics. Exposure to water features such as whirlpools, fountains, and cooling towers has been linked to outbreaks.
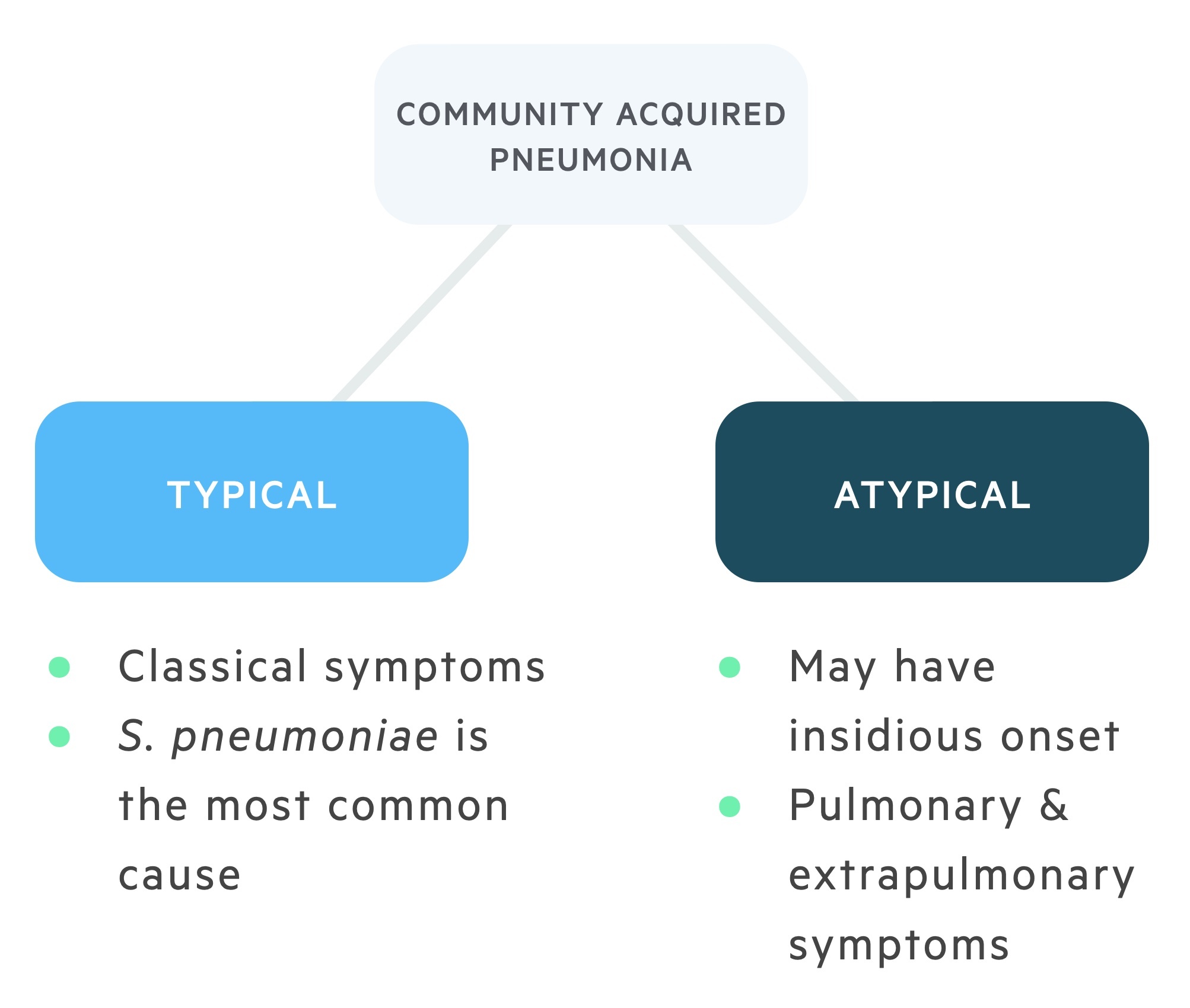
The pneumonia-causing mycoplasma. People under the age of 40 are disproportionately affected by this type of pneumonia. This form of pneumonia is more common among those who live or work in overcrowded environments like dormitories, soup kitchens, and jails. Antibiotics are usually effective against it because it is mild. Mycoplasma pneumonia is a common bacteria but can cause severe illness.
It has been linked to hemolysis and a skin rash. One of the most common causes of “Walking pneumonia” is this particular bacteria. The bacterium Chlamydia pneumonia. In most cases, this mild form of pneumonia can be treated with rest and fluids. Most cases occur in those aged 65 to 79.
In adults, viral pneumonia is most often caused by influenza or flu virus. Among infants younger than a year, respiratory syncytial virus (RSV) is the leading causal agent of viral pneumonia. Rhinovirus, human parainfluenza virus (HPIV), and human metapneumovirus are some other viruses that can cause pneumonia (HMPV).
Viral pneumonia typically manifests as a mild illness. Without treatment, they feel better in two to three weeks. Sometimes, the situation is so dire that it must be handled in a hospital. The likelihood of developing secondary bacterial pneumonia after a bout of viral pneumonia is higher.
Read More: Matt Lucas Illness: Is He Ill? Does the Co-Host of British Actor, Comedian, and Screenwriter?
The Centers for Disease Control and Prevention (CDC) Has Compiled Some Data on Pneumonia Rates in The United States.
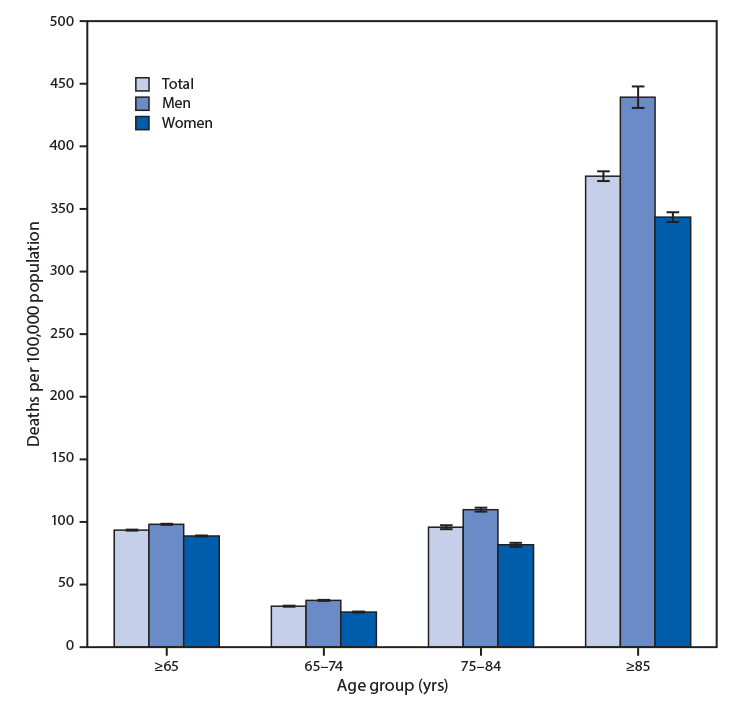
Mortality:
- Annual mortality rate = 48,632
- Among every 100,000 people, 15.1% die.
- 257,000 cases of pneumonia were diagnosed as the primary reason for ER visits.
- Outside of childbirth, pneumonia is the leading cause of hospitalization for adult Americans.
- About one million adult Americans annually seek hospital care for pneumonia.
Vaccination:
- Incidence of pneumococcal vaccination among adults aged 65 and up Pneumonic effusion (69%)
- If fluid builds up too much in the pleural space, this is called a pleural effusion.
- The two main categories of pleural effusion are:
When fluid leaks into the pleural space, it’s called transudative pleural effusion. Caused by either an abnormally high arterial pressure or a low plasma protein concentration. The leading culprit is heart failure.
Causes of exudative effusion include vascular and lymphatic obstruction, inflammation, infection, lung injury, and tumors.
At least 40% of bacterial pneumonia cases also have pleural effusions. They can be broken down into three categories:
A simple parapneumonic effusion is an exudative effusion containing neutrophils that develop when the body produces more pleural fluid than the pleura can reabsorb. As pneumonia improves, so does the condition.
Pleural fluid acidosis, caused by the bacteria’s and neutrophils’ anaerobic metabolism of glucose, is the underlying cause of the complicated parapneumonic effusion.
False-negative results from a culture of this fluid are common, but Gram staining can confirm the presence of bacteria. If fibrin accumulates in the interstitial space between the pleural layers, the fluid may become loculated.
A thoracic empyema is diagnosed when there is pus in the pleural space or when a Gram stain reveals the presence of bacteria. Cultures from 36%-76% of human empyemas contain anaerobic bacteria.
Almost all empyemas and pleural effusions require a drainage procedure in addition to the prescribed antibiotics. Antibiotic treatment alone is usually sufficient to resolve simple effusions, as mentioned above. Pleural effusions can be difficult to drain and may necessitate a tube thoracostomy (chest tube) inserted under CT or ultrasound guidance. Aside from thoracoscopic or open pleural debridement, drainage is the standard treatment for empyema.
Both polyvinyl chloride (PVC) and silicone are frequently used to create thoracostomy tubes. Most have a radiopaque stripe along the length of the tube and fenestrations on the sides of the insertion end. Once in place, the end of the tube will be attached to a pleura-evac machine.
Read More: Ringo Starr Cancels Concert Due to Sudden Illness!
A pleura-evac consists of three distinct chambers—the suction chamber, the water seal chamber, and the collection chamber. A one-way valve, the water seal chamber lets air out of the thoracic cavity and opens in a new tab or window but prevents it from going back in when gravity pulls down.
It may be necessary to implant an ambulatory chest drain device in some patients who have persistent pleural effusion. These gadgets replace the need for a standard drain in the ground with a mechanical, one-way valve. Among these are the flutter valve, flutter bags, chest seals, and stoma bags. They are more manageable in size and make it possible for the patient to walk, eliminating many of the health problems that can arise from bed rest.
